PQA 06 - PQA 06 Biology and Patient Reported Outcomes/QoL/Survivorship Poster Q&A
2839 - SBRT-Induced Tumor Cell Necroptosis Facilitates Immune Evasion by Recruiting MDSCs via the Secretion of CXCL4
Monday, September 30, 2024
5:00 PM - 6:00 PM ET
Location: Hall C
Screen: 19
Zhiyun Liao, MD
Chongqing University Cancer Hospital and Chongqing Cancer Institute
Chongqing, Chonqing
Presenter(s)
Z. Liao1, J. Sui1,2, Y. Wang1,2, and Y. Wu1,2; 1Department of Radiation Oncology, Chongqing Cancer Hospital & Cancer Institute, Chongqing, China, 2College of Medicine, Chongqing University, Chongqing, China
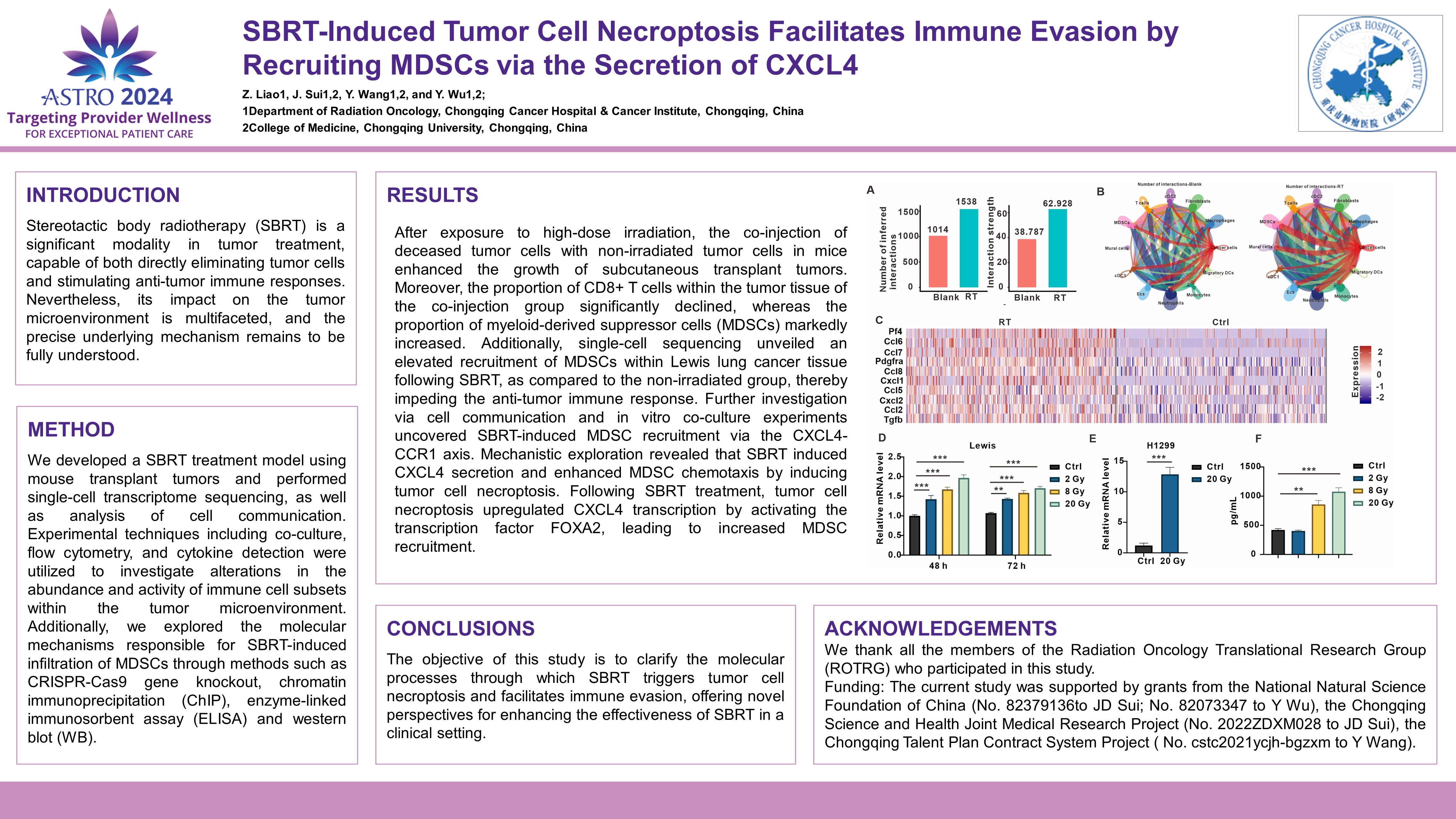
Purpose/Objective(s): Stereotactic body radiotherapy (SBRT) is a significant modality in tumor treatment, capable of both directly eliminating tumor cells and stimulating anti-tumor immune responses. Nevertheless, its impact on the tumor microenvironment is multifaceted, and the precise underlying mechanism remains to be fully understood. Materials/
Methods: We developed a SBRT treatment model using mouse transplant tumors and performed single-cell transcriptome sequencing, as well as analysis of cell communication. Experimental techniques including co-culture, flow cytometry, and cytokine detection were utilized to investigate alterations in the abundance and activity of immune cell subsets within the tumor microenvironment. Additionally, we explored the molecular mechanisms responsible for SBRT-induced infiltration of MDSCs through methods such as CRISPR-Cas9 gene knockout, chromatin immunoprecipitation (ChIP), enzyme-linked immunosorbent assay (ELISA) and western blot (WB).
Results: After exposure to high-dose irradiation, the co-injection of deceased tumor cells with non-irradiated tumor cells in mice enhanced the growth of subcutaneous transplant tumors. Moreover, the proportion of CD8+ T cells within the tumor tissue of the co-injection group significantly declined, whereas the proportion of myeloid-derived suppressor cells (MDSCs) markedly increased. Additionally, single-cell sequencing unveiled an elevated recruitment of MDSCs within Lewis lung cancer tissue following SBRT, as compared to the non-irradiated group, thereby impeding the anti-tumor immune response. Further investigation via cell communication and in vitro co-culture experiments uncovered SBRT-induced MDSC recruitment via the CXCL4-CCR1 axis. Mechanistic exploration revealed that SBRT induced CXCL4 secretion and enhanced MDSC chemotaxis by inducing tumor cell necroptosis. Following SBRT treatment, tumor cell necroptosis upregulated CXCL4 transcription by activating the transcription factor FOXA2, leading to increased MDSC recruitment.
Conclusion: The objective of this study is to clarify the molecular processes through which SBRT triggers tumor cell necroptosis and facilitates immune evasion, offering novel perspectives for enhancing the effectiveness of SBRT in a clinical setting.
Purpose/Objective(s): Stereotactic body radiotherapy (SBRT) is a significant modality in tumor treatment, capable of both directly eliminating tumor cells and stimulating anti-tumor immune responses. Nevertheless, its impact on the tumor microenvironment is multifaceted, and the precise underlying mechanism remains to be fully understood. Materials/
Methods: We developed a SBRT treatment model using mouse transplant tumors and performed single-cell transcriptome sequencing, as well as analysis of cell communication. Experimental techniques including co-culture, flow cytometry, and cytokine detection were utilized to investigate alterations in the abundance and activity of immune cell subsets within the tumor microenvironment. Additionally, we explored the molecular mechanisms responsible for SBRT-induced infiltration of MDSCs through methods such as CRISPR-Cas9 gene knockout, chromatin immunoprecipitation (ChIP), enzyme-linked immunosorbent assay (ELISA) and western blot (WB).
Results: After exposure to high-dose irradiation, the co-injection of deceased tumor cells with non-irradiated tumor cells in mice enhanced the growth of subcutaneous transplant tumors. Moreover, the proportion of CD8+ T cells within the tumor tissue of the co-injection group significantly declined, whereas the proportion of myeloid-derived suppressor cells (MDSCs) markedly increased. Additionally, single-cell sequencing unveiled an elevated recruitment of MDSCs within Lewis lung cancer tissue following SBRT, as compared to the non-irradiated group, thereby impeding the anti-tumor immune response. Further investigation via cell communication and in vitro co-culture experiments uncovered SBRT-induced MDSC recruitment via the CXCL4-CCR1 axis. Mechanistic exploration revealed that SBRT induced CXCL4 secretion and enhanced MDSC chemotaxis by inducing tumor cell necroptosis. Following SBRT treatment, tumor cell necroptosis upregulated CXCL4 transcription by activating the transcription factor FOXA2, leading to increased MDSC recruitment.
Conclusion: The objective of this study is to clarify the molecular processes through which SBRT triggers tumor cell necroptosis and facilitates immune evasion, offering novel perspectives for enhancing the effectiveness of SBRT in a clinical setting.
